Основы нейронаук/Нейродегенеративные заболевания
|
Цели этого урока[править]
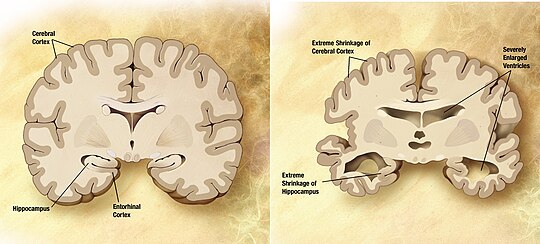 Болезнь Альцгеймера[править]By far the most common neurodegenerative disorder is Alzheimer's disease, which causes increasing memory loss, confusion, and possibly even dementia and death. Alzheimer's is relatively rare among individuals younger than age sixty, however incidence rates of the condition increase exponentially at around this age point, to the extent where nearly half of all individuals aged 85 and older suffer from it. Over the course of the disease, cortical neurons and those in other brain regions (most notably the hippocampus) gradually die as tangled clumps of protein known as senile plaques accumulate. Cognitive declines are the most common criteria for diagnosis, as well as brain scans searching for decay, although the true marker of the disease can only be identified by analysis of brain tissue. This marker is the most commonly implicated cause of the disorder, namely the accumulation of aberrant amyloid and tau proteins into tangles and plaques. These plaques interfere with normal cellular signaling and life processes, leading to the death of neurons. Especially since most of the regions targeted by these plaques regulate cognitive functions and memory, these faculties start to decline. Treatment options for Alzheimer's are still limited though expanding, and are either aimed to ease symptoms or slow- but not halt- degeneration. Drugs can slow the loss of memory by increasing the amount of the neurotransmitter acetylcholine in the brain, while some experimental therapies are attempting to remove the damaging protein plaques. In addition, a wide range of purported preventative measures exist that may help delay the onset of the disease or improve functioning. Болезнь Паркинсона[править] Another common progressive brain disorder is Parkinson's disease, which significantly impairs motor function. Patients with Parkinson's, depending on the progression of their condition, often exhibit muscle rigidity, difficulties walking and performing other basic tasks, and distinctive tremors. Although traditionally Parkinsonism is considered strictly based on motor deficits, in some cases intellectual issues may emerge as well. Genetics only play a role as risk factors for Parkinson's. As for environmental causes, several ideas have been proposed but none conclusively linked. On a neurological level, Parkinson's is linked to neuronal death in a very specific brain region called the substantia niagra. Over the course of aging, neurons naturally tend to die in this brain region and at much higher rates than most other areas. This helps explain why the onset of Parkinson's is so closely tied to aging and why most individuals do not show any symptoms until after about 50 years of age. The substantia niagra is part of the basal ganglia, which accounts for its crucial role in modulating voluntary movement. One of the most widely used treatments to ease the symptoms of Parkinson's is drugs such as Levodopa, which act by boosting dopamine levels in order to compensate for the lost dopamine-producing cells that make up a large part of the substantia niagra. While these drugs have been fairly effective, they by no means eliminate the debilitating motor symptoms and do nothing to halt or slow down the progression of the disease. Rehabilitation and surgical interventions are alternatives still being developed. Рассеянный склероз[править] Multiple sclerosis is an autoimmune disease which leads to a range of neurological symptoms, including impaired motor control, muscle weakness, and loss of coordination, as well as potential mental disturbances such as memory loss or mood changes. Multiple sclerosis has a tendency for varied symptoms as well as varied progressions, with some cases of individuals going through cycles of relapse and remission, and others experiencing steady gradual decline. The condition also emerges at much younger ages than many other degenerative conditions, with onsets usually between the ages of 20 to 40. As an autoimmune disease, multiple sclerosis is caused when an individual's immune system begins attacking healthy body tissues. Specifically, immune cells begin to attack the myelin surrounding axons throughout the nervous system, thereby severely crippling the nervous system's ability to transmit signals. After neurons have their axons damaged in this way, scars (or scleroses) form, which in turn increase the rate of degeneration. The fact that this autoimmune assault may take place anywhere throughout the central nervous system (or, more commonly, in a number of locations at once), the precise symptoms that will result are difficult to predict. For example, degradation of spinal chord axons may contribute to movement difficulties, while in the brain this same degradation may result in psychological consequences. Multiple sclerosis has a fairly strong genetic competent, but what exactly triggers the immune system to start attacking the body is unknown. Treatment options for individuals with this condition is limited, but can counter the effects in a variety of ways. Anti-inflammatory agents can limit the havoc wrought by the immune system, and thus weaken immune attacks and lower the amount of damage done. Medications can also try to fix specific symptoms, such as fatigue or muscle pain. New treatments, especially those which might help neurons repair their damaged axons, are still being developed. |
